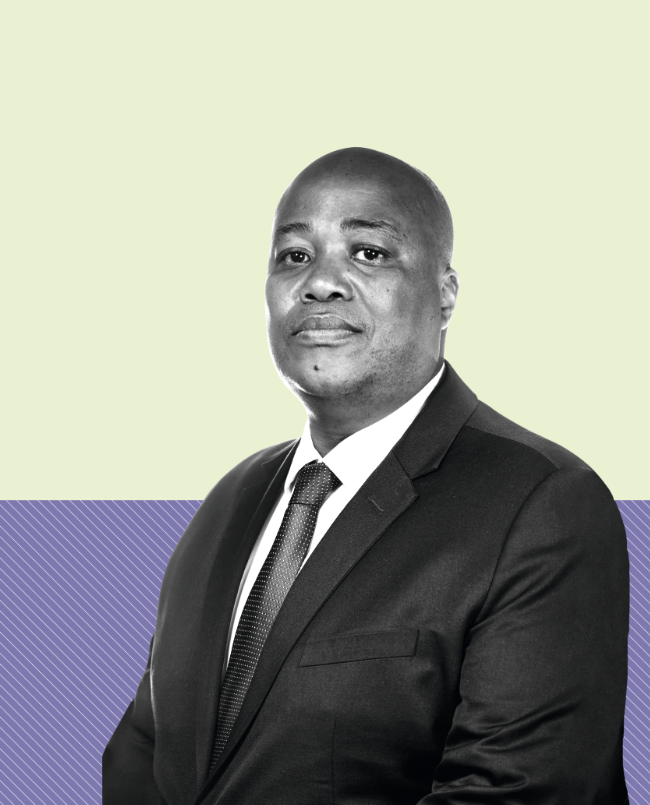
Q: How is it that Growthpoint Properties, more commonly known for its commercial development, has invested in healthcare?
A: The introduction of Growthpoint’s fund management strategy has added depth to the market for broader investment into communities, to further diversify its assets and harness opportunities to create sustainable value. It also allows for others to co-invest in the unlisted and co-invested environment, where there is a differentiation from Growthpoint’s core business.
Two funds were established: the Africa Fund, and the Healthcare Fund. Together the two funds manage assets of some R10 billion and are on track to meet a goal of having around R15 billion by 2023.
We use a ‘capital-light’ model, whereby we raise third-party funding for up to 80% of the capital in each fund and introduce gearing of some 40%. Growthpoint itself invests just 15% to 20% of the capital in each fund, from which it earns distributions.
Q: What are the unique aspects of healthcare and the provision of medical facilities in SA?
A: Healthcare is a defensive sector and assets tend to maintain their earnings and revenues during market downturns, allowing them to perform better than the broader market during a market correction or a bear market accompanied by a recession. Healthcare property leases are also usually long term, which provides institutional investors opportunities to match their long-term liabilities with long-term assets.
Currently, some 84% of South Africans are dependent on the public health sector for their medical needs. Although SA has introduced a number of developments and programmes to improve the delivery of public healthcare, there remains a discord between such provision and patients’ expectations, more so when compared to the private medical facilities and attention given to the sick and injured.
Poorly maintained infrastructure is a further hindrance to SA’s chain of health services in the public sector. Lack of cleanliness and poor maintenance prevail, adding to an unacceptable physical environment.
Q: What are other challenges – and opportunities – in the sector?
A: There is a significant chasm between the quality of healthcare provision in the private and public sectors. This not only relates to bricks and mortar but to healthcare professionals who migrate to the private sector after training, too. The country also loses a considerable number of healthcare professionals to international markets where there are better opportunities.
Private healthcare facilities are concentrated in the larger metropolitan areas and are mostly multidisciplinary, acute facilities. There are therefore opportunities to develop primary healthcare facilities, specialist facilities, day hospitals and provide healthcare in previously under-serviced areas – townships, for example.
Q: How does private and public healthcare positively impact on communities?
A: Full-time and part-time employment opportunities become available during development and operational phases. Training and skills development for healthcare professionals and allied workers also comes into play.
For SMEs there are much-needed hospital support functions, such as security, catering, laundry and so on.
In remote areas, having access to primary medical care is associated with cost-savings for the public, who would not need to travel to the busier city centres for treatment and specialised diagnosis. More benefit comes from being able to treat patients in emergency situations, thereby saving lives. And this has much wider implications in the face of high chronic diseases and, of course, during the COVID-19 pandemic.
The public sector is also known to experience a shortage of specialised equipment, with long waiting lists for surgery or diagnosis, and this potentially exposes them to any number of complications or, worse, loss of life. This is where the private hospitals have the edge, in that their facilities and equipment, through to administrative tools, are acquired when needed as opposed to oft-time lengthy waits by public hospitals for even the most basic equipment, such as scanning machines.
Q: What are the most urgent specialised medical needs, and why?
A: The disease burden in Africa has seen a steady shift from communicable to non-communicable diseases (NCD). The continent has experienced a significant increase in morbidity and mortality related to diabetes, hypertension and other related NCDs with associated cardiovascular disease.
The continent has also witnessed increased morbidity and mortality related to cancer-related illnesses. Mental illness remains a taboo subject in our communities and is significantly under-reported.
The majority of private healthcare facilities in SA are multidisciplinary acute hospitals, and there is definitely a need for more primary healthcare facilities for early detection and management of NCDs, and specialist facilities to address the disease burden.
Q: What plans do you have for new facilities, where will those be and how large is the pipeline of investment?
A: Our Healthcare Fund has a circa R5 billion pipeline comprising acquisitions and development projects. Our development strategy focuses on primary healthcare facilities, day hospitals, specialist facilities and bringing quality healthcare to under-serviced areas.
Too often, these are areas that don’t get the healthcare they need, when they need it. Our future plans include well-considered investments aimed primarily at closing the gaps and strengthening our investment portfolio.
Q: What has been the impact of COVID-19 on SA’s hospital facilities and the health sector in general?
A: In line with global practices, hospitals initially limited surgical procedures to only urgent and emergency cases, with some easing of restrictions to other elective surgical cases under lockdown Levels 4 and 3. This had a significant effect on hospital revenues both from a theatre time and revenue per paid patient day perspective. The healthcare sector has also had to invest significantly in PPE to protect the workforce on the front line of fighting the COVID-19 pandemic.
Field hospitals have had to be hurriedly erected to cope with the forthcoming anticipated peak, which is troubling the health sector deeply because there just isn’t enough equipment to service the infected.
Apart from having to cope with COVID-19, the sector has also had to maintain its services for people who suffer from chronic conditions such as HIV and TB. Programmes that service these prevalent diseases have therefore been disrupted, and this impacts significantly on essential healthcare systems.
Q: What benefits do day hospitals have?
A: Day hospitals offer patients and medical schemes a cost-effective, short-procedure surgical solution without detriment to quality and safety. These include knee, shoulder, elbow, hand, eye, skin, spine, cosmetic, gynaecological, urological, ear nose and throat, as well as dental and general surgery, and a wide range of diagnostic procedures that need to be per- formed in a sterile environment on a same-day-in-and-out basis.
The day-hospital market in SA is small relative to the rest of the world, so there is significant opportunity to grow this market segment.
Q: How transformational is ‘green’ when developing new medical facilities?
A: A green hospital building can be defined as one that enhances patient well-being and aids the curative process while utilising natural resources in an efficient, environment-friendly manner.
Many hospitals and clinics are long-standing landmarks in their communities. Our assets are characterised by long leases, and thus need to be sustainable in order to effectively serve their communities over many decades.
Growthpoint is currently completing the development of the Cintocare head and neck hospital in Menlyn, Pretoria, which is the first green-certified healthcare facility on the African continent.
With this pioneering hospital development also paving the way for a green building certification tool that can be used by others, I do not doubt that SA will see more green-rated hospitals in future.
Q: What is the profile of Cintocare Hospital and how does it change the healthcare landscape?
A: Collaboration between Growthpoint, Cintocare, the Green Building Council of South Africa (GBCSA), Solid Green and Aurecon has manifested in the green certification tool that is considered a road-map to drive the development of new healthcare facilities in SA.
The green rating by the GBCSA was achieved through an architectural approach that incorporates many sustainable design principles. But this doesn’t mean the building is unattractive.
For example, the exterior has green aspects interwoven with sustainability considerations – from its glass facade that serves to shade the building, to design features evocative of the spinal vertebra found in the neck.
Seven floors house the hospital plant room, three clinical and consulting levels, three parking levels for 335 secure parking bays, five theatres (of which three are banked and one a hybrid), and 100 beds, with the capacity to expand up to 160.
Construction, at a cost of R470 million, will be completed later this year and has had input from additional sources such as doctors, promoters, operators and other stakeholders who are keen to be part of the creation of a greener, healthier, more sustainable built environment and improved healthcare sector.